Whether you are at home, an extended care facility, or at home with home health care visits, this time period often brings about questions. Please call us with any questions. We are here to make sure this healing process is as smooth and quick as possible for you.

The First Few Days
Day of Surgery
- Up in chair as tolerated.
- Diet as tolerated. Start slow and advance as you feel better.
- Ankle pumps as instructed.
- Deep breathing with incentive spirometer 10 times every hour while awake.
- Cold compression therapy in place when at rest.
- Physical therapy begins.
- Manage pain.
- Walk with a walker to help with balance for first few days.
- May go up and down a flight of stairs once if needed. Try to limit this as much as possible for the first 2 weeks.
In most cases you will reach all your goals for safe discharge home on the day of surgery. However based on your health, determination of the medical team and your specific needs you may need to spend one night in the hospital for observation.
First Postoperative Day
- If you had knee surgery, the compressive Ace wrap around your knee will be removed. The waterproof banadage over your knee or hip incision will remain in place for 10 days.
- Cold compression therapy in place when at rest.
- Take pain medications as needed.
- Elevate ankle above the knee and the knee above the level of the heart to reduce swelling when not walking or doing your exercises. Do this as much as possible for the first week but at least for 30 minutes 3 times a day. This will help a lot with reducing swelling which will improve your range of motion and pain.
- Do the exercises 3 times a day.
- If you had a knee replacement, keep it moving often. The key is to avoid stiffnesss. Bend your knee joint to 90 degrees and straighten it all the way a few times at least 6 times a day. You can do the exercise to straigten your knee even more frequently to make sure your knee remains straight. You should fully straighten your knee while you are sitting at rest with your leg up whenever you wish to or a few times an hour.
- Stand up and walk a little every hour that you are awake. You do not need to walk far. Limit your steps to less than 750 steps/day in the first week.
- A physical therapist will come to your home to help ensure your are doing well with safe movement and make sure you can do the home exercise program.
- You may shower with assistance.
Second Postoperative Day
- You may notice some more discomfort at your surgery site on this day. Discomfort at the surgery site is typically worse on day 2-5 and then improves each day and week.
- Cold compression therapy in place when at rest.
- Take pain medications as needed.
- Elevate ankle above the knee and the knee above the level of the hart to reduce swelling when not walking or doing your exercises.
- Do the exercises 3 times.
- If you had a knee replacement, keep it moving often.
- Stand up and walk a little every hour that you are awake. Remember, you do not need to walk far. It is just to get all your leg muscles firing a little.
You will settle into a routine and gradually increase your activity level. The key in the first 2 weeks after surgery is managing swelling which is a major contributor pain so your can be comforable after joint replacement. In knee replacement, this is the key to obtaining good range of motion (90-110 degrees) which is your primary goal for the first 2 weeks.
The Incision
Your incision is typically closed in multiple layers with absorbable sutures and then sealed with skin glue. There are no staples or sutures to take out.
The Bandage
There will be a waterproof bandage covering your incision. It is typically clear with a white layer below it. This is a special dressing with silver impregranted into the bandage which protects the incision against bacteria. You may shower with this dressing on as long as it looks sealed against your skin.
You or a caregiver can remove this dressing after 10 days. The incision below is sealed with glue so you do not need to apply another dressing to it.
If you notice any spreading discoloration of the bandage or think there is fluid under the bandage please call us. There should never be any drainage from the incision.
Wound Care
- You may apply moisturizing lotion around the incision with a 1 inch margin. Do not apply any lotion or creams on the incision for the first 6 weeks.
- Do not remove or pull on any scabs. They are a natural part of healing.
- When you shower, let water run over the incision and pat it dry. Do not scrub the incision or try to remove the glue. It will gradually come off over several weeks.
- You can expect to see brusing around your surgery site and your leg. Gravity will pull blood from your surgery site down towards the back of your leg and even to your ankles.
- There should never be any drainage from the incision. If you notice drainage or spreading redness around your incision, it could be a sign of infection.
Warning Signs of Infection
Infection after joint replacement is rare but it is important to watch for any concerning signs so that it can be addressed quickly if happens.
- Increasing redness and tenderness around the incision or bandage.
- Drainage from the incision.
- Increasing knee pain with both activity and rest.
- Persistent fever higher that 101.5. A low grade fever is normal in the first week after surgery and is improved with use to the incentive spirometer and deep breathing.
- Shaking chills.

Your Road to Recovery
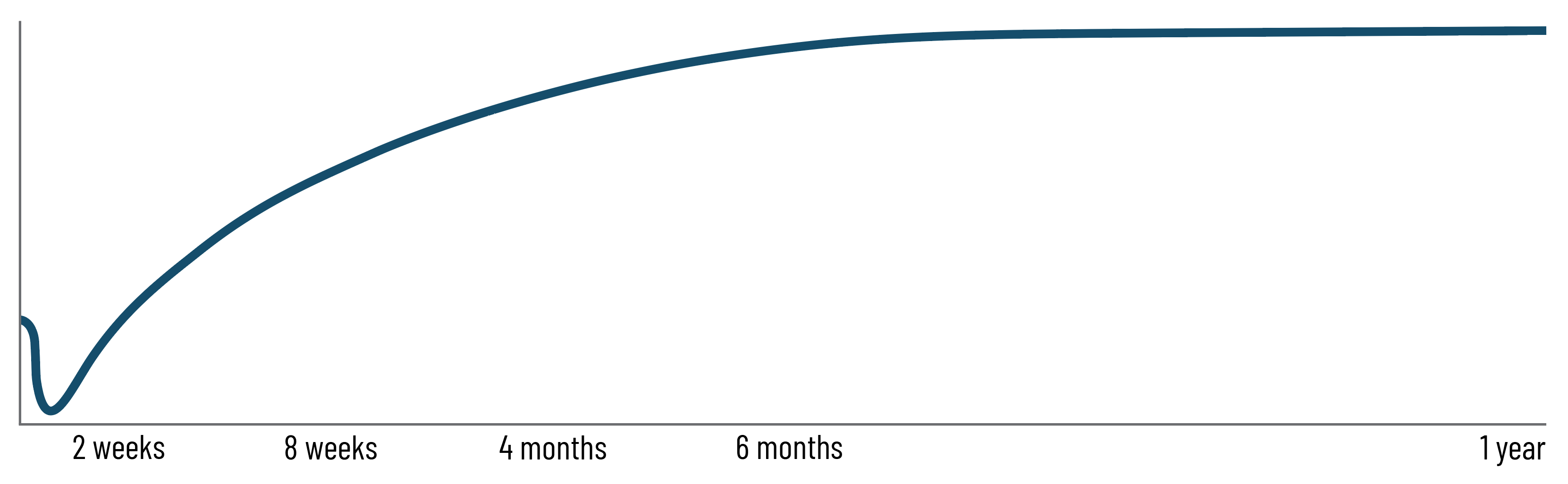
The most intensive part of your recovery from joint replacement happens in the first 2 weeks. You should be able to resume mort normal activities of daily living within 6 weeks after surgery. However, complete recovery takes approximately 6 months. As you become more active during your recovery, it is normal to have discomfort, but it will improve each week. There will always be ups and downs in your recovery. It is important to pace your recovery so that you make steady progress with small ups and downs. Overdoing the exercises to gain strength more quickly, walking too much or doing anything in excess will typically result in setbacks instead of the steady progress expect.
Rehabilitation Exercise Programs
A rehabilitation program is an important part of the recovery after joint replacement replacement. The programs below were carefully designed by Dr. Maratt and physical therapists to help you restore your strength and ability to return to your activities over time.

Rehabiliation after
Hip Replacement
The focus initially is on gait normalization and safe return to activities of daily living.
Week 1 & 2 Full Program
Rehabiliation after
Knee Replacement
Prioritizes early acheivement of full range of motion and then gradual improvement in strength.
Week 1 & 2 Full ProgramDo your exercises for three to four months. Your goal over the next six months, as you become stronger and more mobile, is to gradually replace your exercises with low-impact exercises (walking, biking, elliptical machine).
Walking
You can put full weight on your involved leg (unless specifically told not to) and progress from your walker to a straight cane after 1-2 weeks. Before doing so, make sure you do not have a limp, and be sure you feel safe walking without assistance. You should then use a cane for another 2 weeks or until you feel confident that you wont fall without it.
It’s not uncommon for patients to have a limp prior to surgery and need to really work at not limping or favoring the leg after joint replacement. Your physical therapist can help you with gait training after a few weeks.
While standing facing a countertop or heavy piece of furniture you can hold on to, practice shifting your weight onto the surgery leg. Hold the countertop and lift your surgery leg out to the side with toes facing forward. Then stand on your surgery leg and lift the opposite leg. Do not be surprised if just a few repetitions make your hip tired.
You may gradually discontinue use of your cane. You may find you can walk short distances without assistance at first, but need it for longer trips. As long as you feel safe, do not limp and your pain does not increase, you can use your own judgment about walking without support. However, do not allow yourself to use furniture or walls for support when walking; this means you still need your walking aid. Some patients discontinue their cane or walker after two or three weeks; others need more time. Go at your own pace. There is no strict time limit for using walking aids.
Your safety is the highest priority. Do not discontinue use of a walking aid until you feel confident in your ability to walk without support. A fall early in your recovery can damage your joint replacement.
You may gradually increase how much you are walking in a day. Use the following as a guide:
- Week 1: 750 steps/day maximum
- Week 2: 1200 steps/day maximum
- Week 3: 2000 steps/day maximum
- Week 4: 2750 steps/day maximum
- Week 5: 3500 steps/day maximum
- Week 6: 4500 steps/day maximum
- Week 7+: progress by 1000 steps/day in each subsequent week with pain/swelling as your guide.
Go at your own pace but doing more than the above guidelines may be too much.
Daily Activities
You will need to gradually return to your normal routine. It’s normal for you to feel very tired the first days after surgery, but you need to be out of bed, dressed and moving around at least every hour during your normal awake time. Slowly increasing your activities is most realistic. You can get out of the house when you feel up to it. Walk outside or in an open area such as a mall, go to church, go out to eat or visit friends. Just don’t do it all in one day at first!
During long car trips (more than hour and a half in length), stop every hour or so to get out of the car and walk.
Standing in one place (such as at the sink or stove) might make your hip or knee tired. You may need to sit or walk around for a brief change.
Do not vacuum, mop floors, lift heavy laundry or do strenuous yard work for the first eight weeks after surgery.
Driving
You can drive your car when you can safely and comfortably walk with or without a cane. You must feel safe to get in and out of the car, have good control of your leg and not need opioid pain medication. If you cannot meet all of these criteria, you should not drive.
Other Procedures
Due to the risk of infection, we strongly discourage any non-emergency procedures for 12 weeks following your replacement. This includes dental work, even routine cleaning. We will prescribe an antibiotic that your will take before dental cleanings at your 4 month appointment. Be sure to always tell any health care provider about your joint replacement.


Living With Your Joint Replacement
We encourage you to live a healthy and active life. Exercise should become part of your normal routine. Most people are able to resume low-impact activities such as walking, biking, golfing, swimming and skiing.
Avoid repetitive high-impact activities such as running, high-impact aerobics, jumping, basketball, etc if possible. Anything is ok in moderation but think of your joint replacement as a machine that you want to have last a long time.
Avoid repetitive heavy lifting, such as in assembly line work to the extent possible. Repetitive heavy lifting, every day, all day, can lead to wear and tear on your joint. You may lift heavier weights, such as children, luggage or household items occasionally, as long as you feel safe doing so. Try to carry the weight close to your trunk so you have the best mechanical advantage.
Contents The Day of Surgery Hip Rehabilitation Knee Rehabilitation